Microinvasive glaucoma surgery, or MIGS, offers reduced risks
April 10, 2023

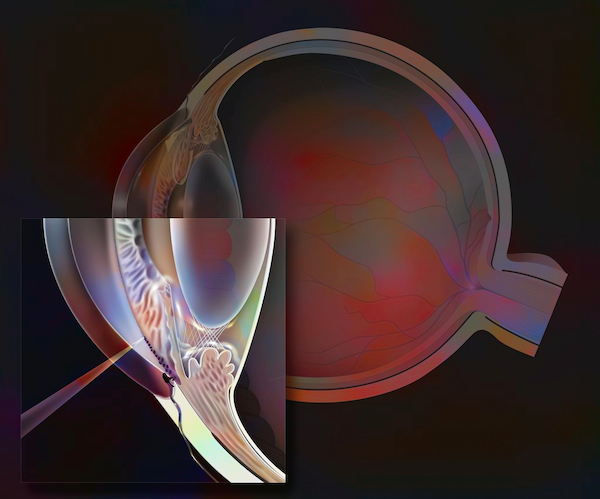
Microinvasive glaucoma surgery (MIGS) is a new type of procedure intended to reduce the risks associated with traditional glaucoma surgery. MIGS is performed with microscopic implants, precision lasers, and tiny incisions in the eye, all of which lead to more rapid healing and visual recovery compared to traditional glaucoma surgery.
Some MIGS procedures are performed as a separate procedure, while others are done at the time of cataract surgery in patients who have visually significant cataracts and glaucoma.
MIGS is an exciting new option for treating glaucoma in select patients, but it does require an experienced glaucoma surgeon, as this field is constantly progressing and improving. It’s important that patients have a glaucoma surgeon who is well versed in all available options as they weigh the benefits and risks of each.
What is glaucoma?
Glaucoma involves progressive damage to the optic nerve, which transmits images from the eye to the brain. Glaucoma affects more than 3 million people in the United States and is usually associated with high pressure inside the eye (intraocular pressure). Patients may develop loss of peripheral vision that can eventually progress to central vision loss and blindness if not properly treated.
In the early stages, most patients have few or no symptoms. As a result, it’s important to have regular eye exams. The American Academy of Ophthalmology recommends having an eye examination:
- Every five to 10 years for people under age 40
- Every two to four years for people 40-54
- Every one to three years for people 55-64
- Every one to two years for people 65 and older or who have glaucoma risk factors such as extreme nearsightedness, African or Hispanic ancestry, a family history of glaucoma, or a thin cornea.
Symptoms of glaucoma can include:
- Loss of peripheral vision
- Halos around lights
- Reduced or cloudy vision
If you develop these symptoms as a result of glaucoma, it is already at an advanced stages. Diagnosing and treating glaucoma early, prior to the development of symptoms, is critical to preventing vision loss.
How is glaucoma diagnosed?
The most common factor associated with glaucoma is high pressure in the eye, but that’s only one risk factor. You can have high pressure in the eye and never develop glaucoma. You can have “normal” eye pressure and have glaucoma.
During a comprehensive eye exam, your doctor might use these common tests to assess for glaucoma:
- Checking your eye pressure
- A dilated-eye exam to view the optic nerve and see if nerve fibers are thinning
- Formal peripheral vision testing called visual field testing
- Optical coherence tomography (OCT) to examine the nerve fibers that feed the optic nerve to look for signs of glaucoma. OCT often helps us diagnose glaucoma earlier than using peripheral vision testing and a clinical examination alone.
Even after testing, we don’t always have a clear diagnosis. There are many patients in the middle ground whom we watch over time to see if their condition progresses into glaucoma.
How is glaucoma treated?
When treating glaucoma, the goal is to reduce eye pressure to prevent further damage to the optic nerve. A patient’s disease stage and lifestyle influence what treatment we recommend, which can include:
- Eye drops, which work to increase the outflow of fluid from the eye.
- Laser treatment, which we use to treat the eye's trabecular meshwork, or drainage system. The procedure increases the flow of fluid from the eye. This can be done in the clinic and typically is not painful.
- Traditional surgery, such as trabeculectomy or tube shunt. With a trabeculectomy, we use the eye’s own tissue to create a new drainage pathway in the eye for fluid to bypass the natural drainage system in the eye, which is not draining enough. With a tube shunt, we implant a flexible drainage tube into the eye to divert fluid inside the eye to an external reservoir. These surgeries have a higher risk profile and are reserved for patients who need that enhanced level of pressure lowering. The patients who need these surgeries typically have a relatively high risk of losing vision because of glaucoma.
- MIGS, which offers less-invasive surgical options to lower pressure inside the eyes. MIGS generally has a more favorable risk profile and might allow surgeons to both reduce pressure and lessen the burden of eye drop use that some patients must rely on.
With traditional glaucoma surgeries, there is a reasonable risk of complications, including:
- Bleeding inside the eye
- Cataract formation
- Decreased vision
- Double vision
- Infection in the eye
- Swelling of the cornea or retina
- Pressure that is too low
Most MIGS procedures have a good safety profile and a more rapid visual recovery, but there is a risk of bleeding in the eye or a short-term increase in eye pressure after the procedure. The specific risks and their likelihood can vary depending on the procedure. At UT Southwestern, my colleagues and I use all of the available MIGS procedures, including:
- iStent: Implanted in the eye’s drainage system, the iStent is about the size of a third of a grain of rice. It creates a permanent opening that improves the eye's natural outflow and lowers and controls pressure within the eye.
- Kahook Dual Blade: A single-use, microengineered blade makes parallel incisions to remove a strip of the eye’s drainage system to improve fluid outflow.
- Ab-Interno Canaloplasty: With this procedure, performed through self-sealing clear corneal incisions, we insert a microcatheter to open the eye’s natural drainage system.
- Endocyclophotocoagulation: Applying laser from inside the eye to the parts of the eye that create fluid, so that less fluid is produced in the eye.
MIGS procedures are relatively new, so we’ll continue to learn more about long-term risks and effectiveness as we follow patients five or 10 years after a procedure. Moreover, new procedures and devices are being developed all the time. It can be difficult to navigate and know what to do, and we are happy to help you explore all options. We offer coverage in all aspects of eye care, so if a patient needs help with other ocular conditions, we can easily connect them with the appropriate specialist.
To learn more about MIGS or talk with an ophthalmologist, call 214-645-2020 or request an appointment online.











