Stereotactic Ablative Radiotherapy (SAbR)/Stereotactic Body Radiation Therapy (SBRT)
SAbR, also known as SBRT, has become a more common treatment that is a particularly robust specialty within our department. Through innovation and clinical testing, clinicians and physicians at UT Southwestern have led its development, which has allowed its safe implementation throughout the field.
SAbR/SBRT is used to treat tumors throughout the body, excluding the brain. Because the technology is so advanced and precise, we can administer a stronger dose of radiation at a time, which means fewer treatments – usually only three to five – and very little healthy tissue receives any radiation.
As pioneers of this specialty, our faculty offers a specialized training course to other medical professionals seeking to gain proficiency in this treatment mode.
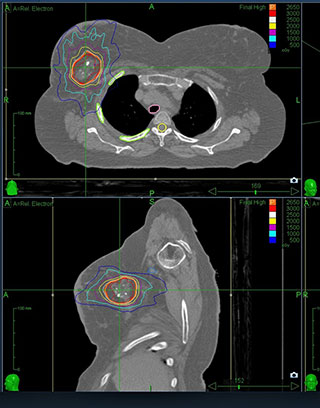
3-D Conformal
Every tumor and patient is different. Using a state-of-the-art computer program, 3-D conformal radiation therapy shapes the radiation beams to match the shape of the tumor. In doing so, we’re able to precisely target the tumor with higher levels of radiation and avoid healthy surrounding tissue. This technique is often used to create a sharp difference between treated and non-treated tissue.
Image-Guided Radiation Therapy (IGRT)
Cancer is often a moving target and anatomy and the size and shape of a tumor can change during the course of treatment. To ensure accuracy, our team uses a variety of imaging tools to match the location of tumors at the time of treatment with the planning location. Imaging tests, such as cone-beam CT scans, are performed in the same room as the patient’s treatment, immediately prior to, during treatment, or both.
Intensity-Modulated Radiation Therapy (IMRT)
This state-of-the-art treatment is a specialized form of 3-D conformal radiation therapy where we’re able to control the intensity of the radiation beam in multiple small volumes to create precisely conformed dose distribution. The radiation beams may be re-shaped dozens or hundreds of times during treatment, resulting in radiation dose distribution that is “sculpted” in three dimensions. Rather than creating a uniform field of radiation, the radiation is delivered to precisely conform to the actual shape of the tumor, thus sparing healthy tissue.
Volumetric Arc Therapy (VMAT) (Varian’s RapidArc)
VMAT is an advanced form of IMRT that delivers radiation while the gantry is moving. Continuous and coordinated changes in gantry speed, dose rate, and shape of the treatment aperture increase deliver treatment speeds to two to eight times faster than conventional therapy, reducing a typical 10- to 15-minute treatment to less than one minute in some cases. Though it doesn’t reduce the total number of treatments patients require, the duration of each treatment is shorter which makes it more convenient for patients who must undergo multiple treatments. VMAT is particularly useful when delivering radiation near sensitive organs. Prostate and head and neck patients are often candidates for VMAT therapy.