What if you could do something today that could spare your child from developing cancer in adulthood? You’d do it, wouldn’t you?
The HPV vaccine could give parents that chance, possibly preventing in their kids today the development later in life of certain types of head and neck cancer.
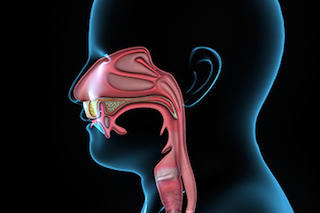
HPV – the human papillomavirus – is best known for causing cervical cancer in women, but it can also cause types of head and neck cancers. Other head and neck cancers are caused by smoking or chewing tobacco, drinking alcohol, or having a poor diet. What’s alarming is that while the national trend for these other head and neck cancers is going down, we’re seeing a tremendous increase in the types of head and neck cancer caused by HPV infection.
Around 9,000 people each year are diagnosed with cancer in the oropharynx – areas in the throat including the base of the tongue and tonsils – that may be caused by HPV. This statistic indicates that HPV-related head and neck cancer is an epidemic.
What is HPV-related cancer?
HPV is an extremely common sexually transmitted infection. Over 95 percent of sexually active adults contract HPV at some point in their lives, many without even realizing they have it. Often, the infection goes away on its own without causing long-term issues. But 30 percent to 40 percent of adults contract high-risk HPV, which means they contract HPV strains that are known to cause cancer.
Head and neck cancer patients used to be, on average, 60 to 70 years old, and often their cancer could be attributed to substance abuse – specifically to smoking and excessive alcohol use. Today, we’re seeing patients in their 30s to 50s who lead healthier lifestyles but have developed HPV-related head and neck cancer.
Symptoms of HPV-related cancers affecting the oropharynx may include persistent sore throat, earaches, hoarseness, enlarged lymph nodes in the neck, pain when swallowing, and unexplained weight loss. Though HPV infection is not gender specific, HPV-related head and neck cancer is four times as prevalent in men.
There’s no screening exam or straightforward process – like a PAP smear for cervical cancer – to check for HPV-related throat cancer. Current screening tests are not accurate enough to pick up the early, very small tumors caused by HPV infection.
Vaccinate your kids against HPV
In recent years, the HPV vaccine has been recommended for preteens as protection against cervical cancer and other genital cancers. Many parents do not know that one of the cancers the vaccine could also prevent is HPV-related head and neck cancer.
Adolescent uptake of the 3-dose HPV vaccine series is 38% – far below our national goal of 80%. Though it could keep their son or daughter from developing HPV or HPV-related genital cancer as an adult, some parents feel uncomfortable vaccinating 11- and 12-year-olds against a sexually transmitted infection.
But as I mentioned, the majority of sexually active adults will contract HPV in their lifetimes. Once HPV exposure occurs, there’s no good way to prevent infection if you have not been vaccinated. For this reason, it would be wise for parents to think very seriously about vaccinating their kids against HPV.
The HPV vaccine works to protect against HPV-related genital cancers, so it makes sense that it would also help prevent HPV-related head and neck cancer. The HPV strains that cause genital cancer and head and neck cancer are the same – HPV 16 and 18.
Right now, the HPV vaccine has not been proven to prevent HPV-related head and neck cancer, partly because it takes decades to develop this cancer and we don’t have tests to detect head and neck precancers early. Over the next 20 years, we will be following the progress of kids who have been vaccinated to see if the number of HPV-related head and neck cancers drops just like the number of cervical precancers.
How is HPV-related cancer treated?
The prognosis for HPV-related head and neck cancer is usually good. We typically see over 90 percent cure rates, even including advanced stages of the disease.
But that doesn’t mean it’s something to take lightly. It’s still cancer, and you really don’t want to get it. I have cared for patients with metastatic cancer brought on by HPV, and it can be deadly.
If you receive an HPV-related head and neck cancer diagnosis, surgery is often the cornerstone of therapy along with radiation and chemotherapy. For these cancers we typically perform minimally invasive robotic surgery to remove as much of the tumor as possible. This potentially allows us to de-intensify the amount of radiation we have to give you, and about half the time we can avoid chemotherapy, even for advanced disease.
Our research team is continually thinking of ways to decrease the long-term side effects of cancer therapy. That’s especially relevant for HPV-related cancers because patients are often young and in the prime of their lives. We don’t want patients to have to deal with the common side effects from oropharyngeal radiation therapy, which can affect teeth, speech, swallowing, and breathing in the many years to come.
One question we hear from patients is, “Since HPV is a sexually transmitted infection, why did my partner develop cancer but I didn’t?” Honestly, we just don’t know the answer to that yet.
What we know is infections and cancer affect people differently. Recent studies suggest that though HPV itself is contagious, HPV-related head and neck cancer does not appear to be. In other words, you do not need to worry about transmitting HPV-related cancer to your partner.
Talk to your kids’ pediatrician about vaccinating them against HPV. The vaccine is proven to protect them from HPV infection and cervical cancer – and it could very likely protect them from HPV-related head and neck cancer, too.

www.cdc.gov











