Can you turn a breech baby around?
December 29, 2015
Celebrity pregnancies are often hot entertainment news. In December 2015, breech babies got their 15 minutes of fame when Kim Kardashian announced that she had undergone external cephalic version (ECV) to rotate her baby from a breech position to a head-down position.
But what is breech, what does it mean for you and your baby, and what can you and doctors do about it?
What is a breech baby?
Breech means that the baby’s bottom or feet are in the lower portion of the uterus, over the cervix. In a normal delivery position, the baby’s head is down, allowing it to be delivered first. Almost all babies are breech at some point of the pregnancy, but by 37 weeks, 96 percent of babies will naturally be in a head-down position.
There are three types of breech positions:
- Frank breech: The baby’s bottom is down and the legs are up in front of the face.
- Complete breech: The baby’s bottom is down with the legs folded cross-legged.
- Footling breech: The baby’s legs are extended below the baby’s bottom.
There are multiple reasons your baby might be in the breech position at the end of the pregnancy. Sometimes there is no cause; think of it as your baby’s first moment of stubbornness! These are some common reasons:
- Multiple babies
- Too much or too little amniotic fluid
- An abnormally-shaped uterus
- Placenta previa, in which the placenta is partially or completely covering the cervix
Using external cephalic version to turn a breech baby
If your baby is still breech between 36 and 38 weeks, we can try ECV to try to turn the baby to a head-down position. ECV has a 50 percent to 60 percent success rate. However, even if it does work, there is still a chance the baby will return to the breech position before birth.
ECV is done in labor and delivery at the hospital, not in an office setting. We do it there in case the procedure stimulates labor or the baby shows signs of distress and we need to deliver immediately. We monitor the baby’s heart rate the entire time.
Before the procedure, we will do an ultrasound, and we might give you a shot to help your uterus relax. ECV isn’t comfortable, but it shouldn’t be terribly painful. Your doctor can walk through whether an epidural may be right for you.
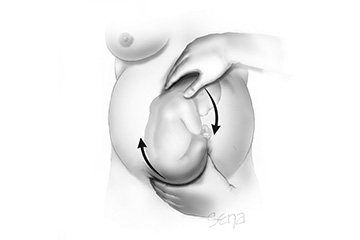
Next, almost like a massage, we use both hands – one by the baby’s head and one on the rump – to attempt to push and roll the baby into a head-down position. It’s sort of like a forward somersault for the baby. The whole process should take 45 minutes or less, and your baby’s well being is monitored throughout the procedure.
The risks of ECV are low, but can include:
- Rupturing the amniotic sac and beginning labor, which may require a cesarean section
- Placenta abruption, in which the placenta separates from the uterus before delivery
- Twisting or squeezing the umbilical cord, which would reduce blood flow and oxygen to the baby
Using chiropractic and acupuncture methods
While external cephalic version is an obstetric technique, there are a few chiropractic and Eastern medicine methods that have shown some evidenced-based success in getting breech babies into the correct position.
Webster technique: Larry Webster, founder of the International Chiropractic Pediatric Association, developed this method in 1978 to adjust the sacrum, the large triangular bone at the base of the spine, to relieve intra-abdominal muscle tension and align the pelvis so the baby can turn naturally. In this technique, the chiropractor is not manipulating the baby, but instead the mother’s spine.
A Journal of Manipulative and Physiological Therapeutics survey of chiropractors in 2002 showed there was an 82 percent success rate of babies turning from the breech position when the Webster technique was used between 32 and 35 weeks. This method is used pretty early, so I think the chances are good that these babies would turn naturally without it. However, it is safe, so there’s nothing wrong with trying it.
Acupuncture combined with moxibustion: This method is based on the thought that stimulating an acupuncture point on the outside of the pinky toe increases fetal activity, and therefore increases the likelihood of the baby turning. However, there are no randomized control trials looking at acupuncture by itself in getting a baby to turn from the breech position.
Moxibustion is the burning of an herb called moxa (more commonly known as mugwort) near an acupuncture point. A 1998 study in the Journal of the American Medical Association compared two groups of women whose babies were breech at 33 weeks: One group received no interventions while the other group received acupuncture combined with Moxibustion. At 35 weeks, 75 percent of the babies in the Moxibustion group were no longer breech, compared with 45 percent in the control group.
Can you turn a breech baby on your own?
If you Google “How to turn a breech baby,” you’ll find all sorts of “advice” for home interventions. Patients often ask me about techniques they read about on the Internet. At 32 to 34 weeks, there is plenty of time for babies to turn on their own. At that point in the pregnancy, I recommend you simply exercise patience. However, while these techniques do not have evidence-based data to prove they work, some of them are safe and there’s no reason why you can’t try them. Here are a few that my patients have asked me about:
- Pelvic tilting: Lie down on the floor with your pelvis raised on pillows a few times a day. While this may not work to turn your breech baby, it may make your back feel better!
- Headstands in a pool: This may sound crazy, but some people are convinced it works. As long as you are comfortable in the water and can hold your breath, feel free to give it a try.
- Playing music near your pubic bone: The thought is if you play music or have your partner talk near the pubic bone, the baby will respond to the sound and turn toward it.
- Cold pack and heating pad: Some people believe that putting a cold pack toward the top of your belly and a heating pad near the pubic bone will encourage the baby to turn. However, your baby is encased in fluid, and it takes a lot to heat or cool a body of water, so this is probably not going to accomplish anything other than making your skin hot and cold.
One technique I do not recommend is rubbing peppermint essential oil on your belly. Constantly covering your belly with the oil can cause skin irritation, trigger an allergic reaction, or, depending on how much is absorbed, change the activity of enzymes that metabolize certain drugs.
Delivering a breech baby
Most healthcare providers will recommend a C-section if your baby is breech when you go into labor. While Clements University Hospital does allow vaginal breech delivery if the patient is a good candidate, some hospitals do not allow planned vaginal breech deliveries. With a breech birth, the baby’s head is the last thing to come through the birth canal, which makes it more difficult to ease it through, leading to the possibility it may become trapped. Another risk is cord prolapse, in which the umbilical cord is squeezed as the baby moves toward the birth canal, slowing the baby’s supply of oxygen and blood.
The Your Pregnancy Matters blog publishes new stories about pregnancy, labor, and delivery every Tuesday. Sign up to receive an email when new stories are published.
C-sections have been shown to have better outcomes for breech babies. The Term Breech Trial was an international study in which half the women had a planned C-section and half had a planned vaginal delivery. For developed countries like the U.S., the benefits of a C-section were fairly significant, with a 0.4 percent risk of the baby dying with C-section compared with a 5.7 percent risk with vaginal delivery.
In 2006, the American Congress of Obstetricians and Gynecologists wrote an opinion that C-sections should be preferred in most situations, when a baby is breech. They also said that depending on the experience of the healthcare provider and hospital protocols, vaginal delivery could be considered, but it is important to discuss the risk factors with the mother.
If having a vaginal delivery is important to you, discuss it with your obstetrician or certified nurse midwife, and listen closely to what they advise. A healthy baby and a healthy mom ultimately is everyone’s goal.











